The ubiquity of respiratory diseases – like asthma, bronchitis, and lung cancer – across the world necessitates accessible, easily-handled treatment methods that work effectively and at low costs. As highlighted in a recent article by ME Associate Professor Jesse Capecelatro, “aerosol administration has emerged as a viable treatment capable of delivering as much as 100 times higher drug concentrations to a patient’s lungs when compared to systemic or oral delivery.” In practice, however, the devices for aerosol administration (i.e., dry powder inhalers) have difficulty meeting this potential.
Dry powder inhalers (DPIs), comparable to “metered dose inhalers” commonly used to treat asthma, are usually packed with very fine, light pharmaceutical powder. This causes trouble when a powder, bearing a similar consistency to powdered sugar, encounters moisture on the walls of the mouth and throat. Much of the fine, loose powder becomes stuck, resulting in – a keyword throughout Dr. Capecelatro’s article – mouth-throat (MT) depositional loss: the percentage of drug that does not reach a patient’s lungs (in the way of 40-80% for “most DPIs intended for properly trained adults”). The trouble here, Dr. Capecelatro told us, is turbulence, a fluid motion characterized by chaotic changes in flow velocity.
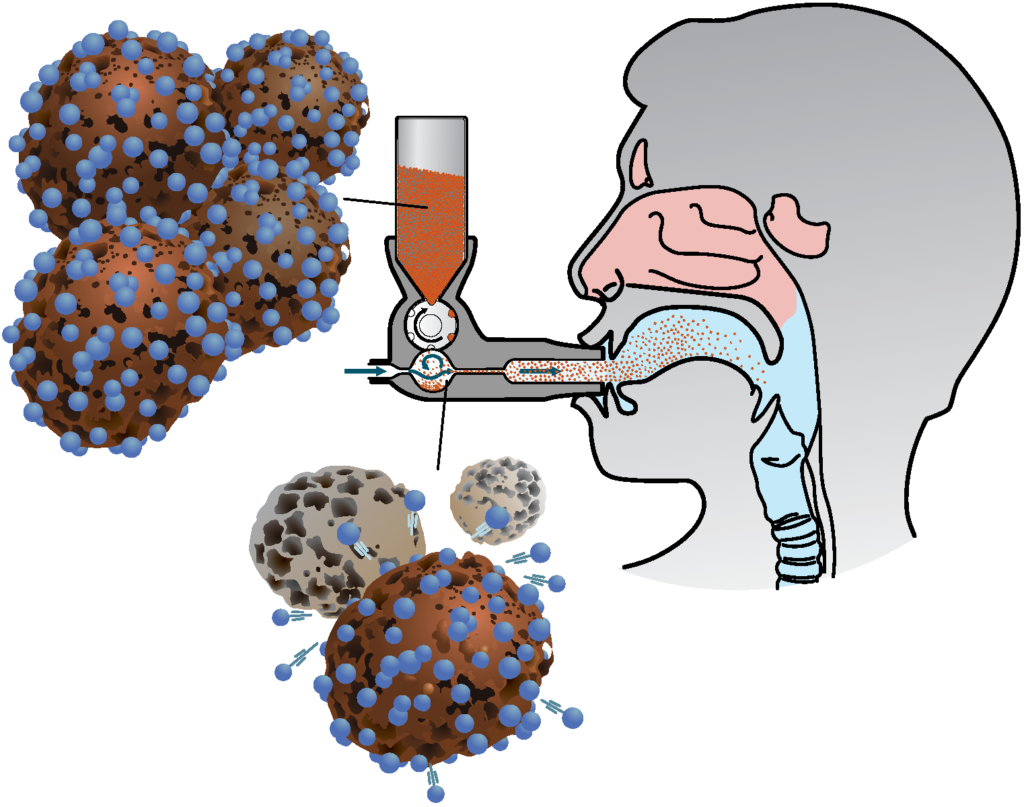
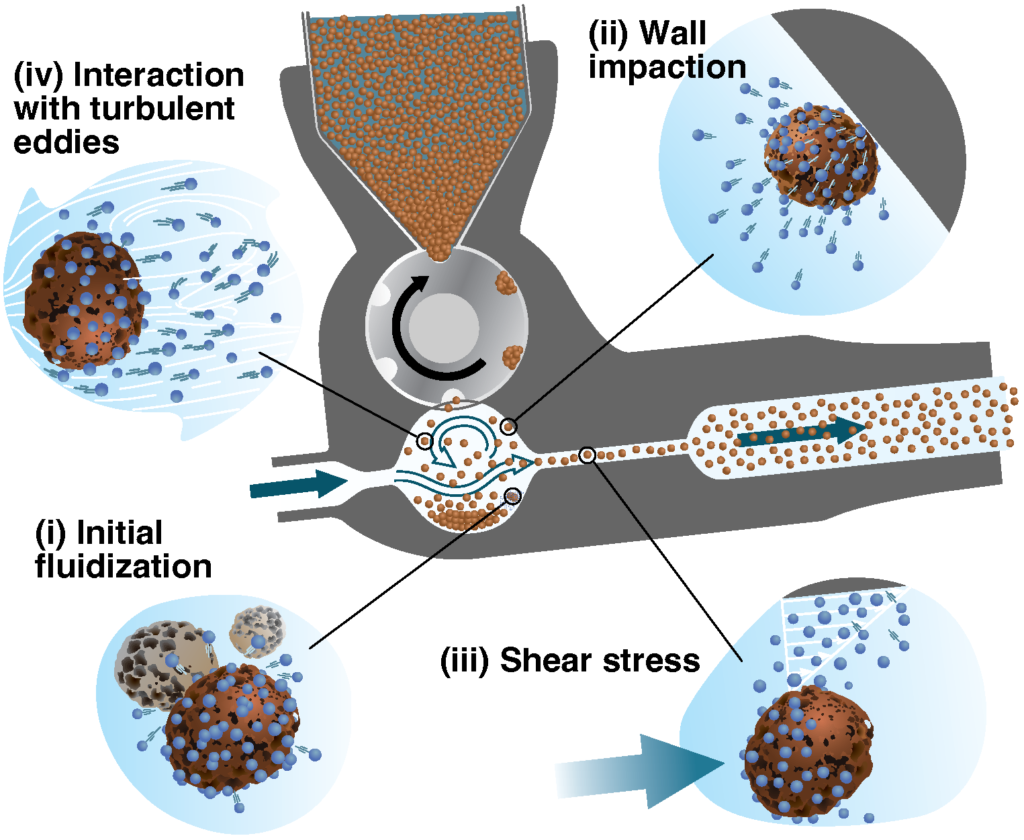
DPIs rely on turbulence to “fluidize” pharmaceutical particles so that they disperse into a patient’s respiratory tract, and eventually reach the lungs. To minimize depositional loss, turbulent flow must be strong enough to drive the powder, initially packed down at the base of an inhaler, up through the mouthpiece, but then weak enough not to scatter the light drug particles throughout a patient’s mouth and throat. This is more easily said than done.
Achieving the ideal flows for effective drug delivery is complicated by several factors that vary from drug to drug and from patient to patient, including mouthpiece size and fit, the length and width of a patient’s respiratory tract, and the size and shape of the particles of the drug an inhaler will administer. These complexities pose a significant hurdle for the drug delivery community to model, a practice necessary for effective design. Outside of the drug delivery community, however, recent advancements in computational modeling have opened new avenues.
Advanced Drug Delivery Reviews, a peer-reviewed journal, invited Dr. Capecelatro and his collaborators to write an article that amplifies recent computational modeling techniques that could be very useful to those in the drug delivery community in designing DPIs. The article’s intention, Dr. Capecelatro told us, was to say “here’s what the state of the art is. It hasn’t yet been used to model dry powder inhalers, but it should be.” The article ultimately presents criteria for designing an “ideal inhaler,” that it should be drug- and patient-specific, which poses a serious cost and accessibility problem.
API particles and subsequent dispersion.
Efforts to model air flow and track drug particles for specific drugs and patients are often costly. Computational fluid dynamics (CFD) that solves for both the air flow and particles have tradeoffs in terms of speed and accuracy. Detailed simulations that track each individual particle and fully resolve the turbulent flow field must be done on supercomputers and can take days, weeks, or even months to complete. Simplified models can be performed on a laptop in much faster time, but fail to capture much of the key aspects taking place in a DPI. Much research done today seeks to develop capabilities to simulate such flows with the accuracy of detailed calculations but at the cost of simplified models.
Most often, the main focus of the computational models in question is airflows and how they affect the trajectory of drug particles. As Dr. Capecelatro argues, this neglects several factors, like how particles interact with each other and affect flows. One solution specifically offered in the article is to couple CFD with discrete element modeling (DEM), so that models account for “the multiple forces acting on [drug] particles.” “Detailed CFD-DEM simulations are valuable as they can provide insights into the dominant disaggregation mechanisms in a DPI, along with a spatiotemporal map of the evolution of the extent of disaggregation.”
In all, there are a range of options available to DPI designers for problem-solving through the complexities of achieving appropriate flows for each drug and patient. “I’ve watched and participated in these advancements in computational modeling for so long, but we rarely get to see the end-user, outside of academia, benefit from that. That’s what I’d like to see: someone who’s designing a dry-powder inhaler being able to benefit and make use of these advancements,” said Dr. Capecelatro.
With the appropriate university credentials, you can read more by following this link: Recent developments in the computational simulation of dry powder inhalers.
