After having received a $50,000 grant from MCubed—a seed funding program at the University— a research project to develop an innovative biochip platform for advanced immune status monitoring has been awarded additional funding this July. This funding, given by the National Institutes of Health (NIH), has brought the interdisciplinary team one leap closer to testing the immune monitoring biochip in a clinical setting and improving patient care.
A team of clinical practitioners and ME professors coordinated their studies about three years ago. ME Professor Jianping Fu, ME Professor Katsuo Kurabayashi, Timothy T. Cornell, and Thomas P. Shanley collaborated on the research after the clinical sector expressed the need for a more efficient and informative immunology test. Cornell and Shanley both specialize in Pediatric care and Fu and Kurabayashi work within the ME department.
“Our clinical collaborators found us, in fact, because there’s a critical need for improved bed-side assays that can afford rapid and accurate determination of patient immune status,” Fu said. “This is particularly important for neonatal or pediatric patients in the intensive care unit, as they don’t have a lot of blood to give for conventional, existing tests.”
According to Fu, the diversity of the team member’s areas of study was a significant factor considered by MCubed before the NIH grant was awarded.
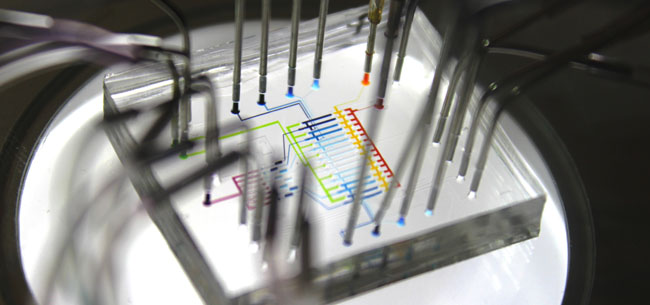
“We have a lot of experience in microscale sample preparation, useful for handling complex body fluids such as blood,” Fu added. “Katsou’s renowned expertise in optical detection and biosensing plays also a critical role for this integrated biochip platform.”
The researchers were allowed to expend the MCubed funding according to their own specialized agenda.
Microfluidic immunophenotyping research team. (from left to right) Xiang Li, Bo-Ram Oh, Zeta Yu, Jianping Fu, Timothy T. Cornell, Katsuo Kurabayashi, Thomas P. Shanley, Nien-Tsu Huang (now assistant professor at the National Taiwan University), and Weiqiang Chen (now assistant professor at the New York University)
The progress made in research supported by MCubed opened up new doors of opportunity for the project, once it became eligible for a $3 million NIH grant. Last July, the NIH grant money was awarded and will be dispersed over the next four years to allow the team to apply and test their immune monitoring biochip in the clinical setting.
“The MCubed grant was really helpful because it supported our initial research effort and allowed us to produce preliminary results that were needed for bigger NIH funding,” Fu said.
The conventional method of testing the immune status of patients requires a large amount of blood, which can pose a problem for infants and neonates whose bodies contain only tens of milliliters of blood. Additionally, conventional methods take twenty-four hours to produce results. This delay significantly slows down clinical decision making, which can ultimately detriment patients, especially those with sepsis, that need urgent care.
The new biochip takes a smaller amount of blood, processes it in just an hour, and analyzes it on a more detailed scale. As opposed to assessing the blood sample as a whole, the new platform is able to separate immune cells by type, measuring the function of each one.
“We have strong expertise in developing an integrated platform that allows us, for example, to isolate different immune cells and examine their function simultaneously,” Fu said. “We hope our approach can allow our clinical collaborators to identify the immune cell types that are responsible for dysregulation of patient immune system.”
For patients susceptible to sepsis or who have undergone an organ transplant it is important that each subset of the immune cells is analyzed so that the patient can retain minimum immune function.
With the NIH grant, the research team is now ready to apply their immune monitoring biochip to identify patients in the intensive care unit that are more susceptible to infection and sepsis. They are also collaborating with University doctors to apply their technology for titration of dose of immunosuppressive drugs given to patients who have undergone an organ transplant.

